- Scientific Basis of Inflammation-First Knee Arthritis Care
This page summarises the scientific evidence supporting an inflammation-first approach to knee osteoarthritis, as presented in the Inflammation Pillar Video. Each section corresponds directly to a key statement from the script, supported by peer-reviewed research.
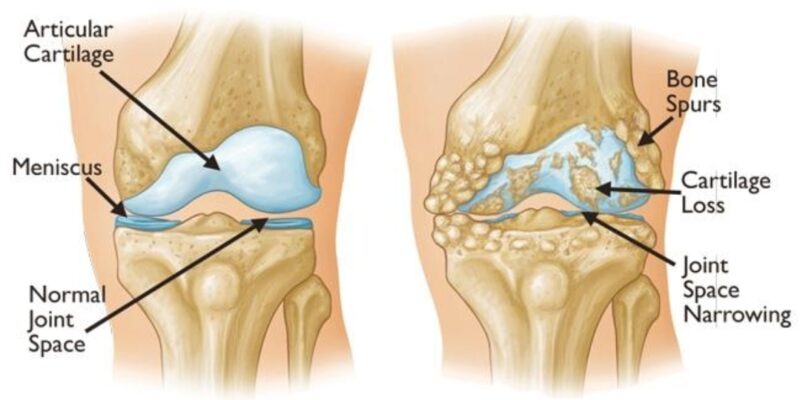
1. Knee Arthritis Is Not Just Wear and Tear
Scientific Proof
Osteoarthritis is now recognised as a whole-joint inflammatory disease involving the synovium, cartilage, subchondral bone, ligaments, and infrapatellar fat pad.
Key References
- Robinson WH et al., Nature Reviews Rheumatology – Osteoarthritis as an inflammatory disease
- Berenbaum F, Osteoarthritis and Cartilage – Low-grade chronic inflammation in OA progression
Consensus
Mechanical damage alone does not explain pain severity or disease progression.
2. Inflammation Inside the Joint Drives Pain, Stiffness, and Progression
Scientific Proof
- Synovitis strongly correlates with pain severity
- Associated with effusion and stiffness
- Predicts faster cartilage loss
Key References
- Hill CL et al., Annals of the Rheumatic Diseases
- Felson DT et al., Arthritis & Rheumatology
Consensus
Pain tracks inflammatory activity, not X-ray grade.
3. Two Patients With the Same X-Ray Can Have Very Different Pain
Scientific Proof
Radiographic severity correlates poorly with clinical symptoms.
Key References
- Bedson J, Croft PR, Rheumatology
- Hannan MT et al., Arthritis & Rheumatism
Consensus
Imaging underestimates biological disease activity.
4. Exercise Improves Support, Not Inflammation
Scientific Proof
- Improves muscle strength and neuromuscular control
- Does not suppress synovial cytokines when inflammation is active
Key References
- Henriksen M et al., Osteoarthritis and Cartilage
- Baker KR et al., Arthritis Care & Research
Consensus
Exercise is necessary but biologically insufficient when inflammation is uncontrolled.
5. Why Patients Plateau Despite Good Physiotherapy
Scientific Proof
- Active synovitis predicts poor rehabilitation response
- Associated with pain flares after loading
- Reduces tolerance to strengthening
Key References
- Scanzello CR et al., Clinical Orthopaedics and Related Research
- Schaible HG, Nature Reviews Rheumatology
Consensus
Plateaus are biological, not motivational failures.
6. Painkillers Suppress Symptoms, Not Disease Biology
Scientific Proof
- NSAIDs reduce pain temporarily
- Do not halt cartilage degeneration
- Do not modify disease progression
Key References
- Zhang W et al., OARSI Guidelines
- Hochberg MC et al., Arthritis Care & Research
Consensus
Symptom relief does not equal disease control.
7. Sequence Matters: Calm Inflammation Before Strengthening
Scientific Proof
- Reducing inflammatory load improves pain thresholds
- Improves exercise tolerance
- Enhances functional outcomes
Key References
- Atukorala I et al., Arthritis Research & Therapy
- Bennell KL et al., British Journal of Sports Medicine
Consensus
Biological readiness determines rehabilitation success.
8. Joint Preservation Focuses on Biology, Not Just Mechanics
Scientific Proof
Modern OA management emphasises early biological modulation, load management, and individualised treatment sequencing.
Key References
- Loeser RF et al., Osteoarthritis and Cartilage
- Hunter DJ, The Lancet
Consensus
Joint preservation is proactive, not passive.
9. Inflammation Is Treatable
Scientific Proof
- Inflammation in OA is measurable
- Inflammation is modifiable
- Inflammation is clinically meaningful
Key References
- Mathiessen A, Conaghan PG, Arthritis Research & Therapy
- Scanzello CR, Goldring SR, Arthritis & Rheumatology
Consensus
Osteoarthritis inflammation is manageable, not inevitable.
See the video here -https://youtu.be/IJFPdKUwpc0?si=5lN4781-zEmo3Xk0
FAQ’s
Q: Is knee osteoarthritis only caused by wear and tear?
A: No. Current research shows osteoarthritis is a whole-joint inflammatory disease. Mechanical wear alone does not explain pain severity or progression.
Q: Why does knee pain not match X-ray findings?
A: Pain correlates more strongly with synovial inflammation than with radiographic cartilage loss. X-rays underestimate biological disease activity.
Q: Does exercise reduce inflammation in knee arthritis?
A: Exercise improves strength and support but does not reliably suppress active synovial inflammation when it is present.
Q: Why do some patients plateau despite physiotherapy?
A: Active inflammation sensitises pain pathways and limits tolerance to loading, leading to biological—not motivational—plateaus.
Q: Are painkillers disease-modifying in knee arthritis?
A: No. NSAIDs reduce symptoms temporarily but do not alter the underlying disease process or progression.