A-Kavach™ – The Biological shield That Protects Your Joints From Arthritis
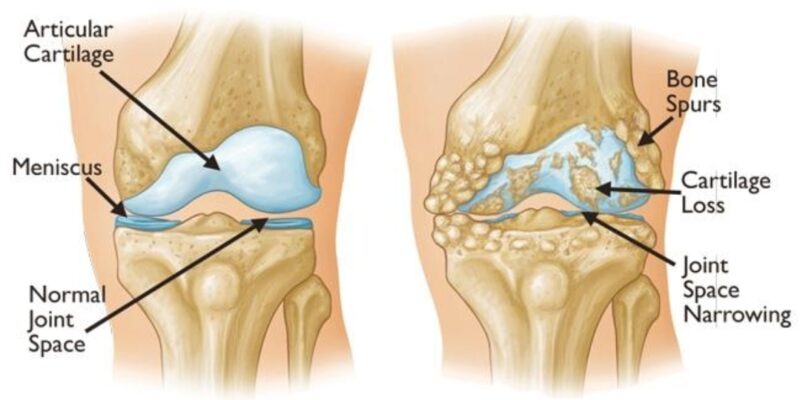
Arthritis is not just “wear and tear.” For decades, patients were told that their cartilage simply eroded because of aging or excessive load. But modern mechano-biologic science reveals a much more complex—and more important—truth:
Your knee is under a chemical attack.
Inside an arthritic joint, destructive enzymes (proteases), inflammatory molecules, and oxidative stress behave like microscopic knives, cutting through cartilage and accelerating degeneration. Even if your X-ray looks “mild,” the chemical destruction can be severe.
A-Kavach™ is designed to stop this destruction before true damage occurs.
Why the Old “Wear and Tear” Theory Is Outdated
For years, osteoarthritis was explained only as a mechanical problem. But today we know that:
- Cartilage breakdown is driven by biochemical inflammation
- Specific enzymes—MMPs, ADAMTS, and cytokines—dissolve collagen and proteoglycans
- These changes start silently, long before severe X-ray findings
- This is why some patients with “normal” X-rays have severe pain
- And some people with terrible X-rays have no pain at all
Mechanical load alone does NOT cause arthritis. Chemical assault does.
A-Kavach™ is built specifically to interrupt this chemical cascade.
What Is A-Kavach™?
A-Kavach™ is a biological defence protocol designed at Madras Rejuvenation Centre to protect your cartilage from the destructive forces of osteoarthritis.
It works through a 3-layered mechanism:
1. Shielding the cartilage from destructive enzymes
Biologic agents used in A-Kavach™ neutralize excess proteases and inflammatory molecules. This slows the chemical erosion that silently eats away at cartilage.
2. Improving joint biology and nutrient flow
Healthy cartilage depends on movement, pressure gradients, and cellular health. A-Kavach™ restores the biological environment needed for repair.
3. Reducing pain generators inside the joint
Pain signals come from:
- Synovial inflammation
- Bone marrow lesions
- Nerve sensitization
- Piezo-mechanoreceptor dysfunction
A-Kavach™ addresses these pain pathways to restore comfort and confidence.
Who Is A-Kavach™ For?
A-Kavach™ is ideal for patients who:
- Have early to moderate osteoarthritis
- Experience pain not explained by X-ray severity
- Want to avoid or delay knee replacement
- Have active inflammation inside the joint
- Prefer a PR to joint preservation
- Want to maintain mobility and function for years to come
Patients with metabolic syndrome, obesity, or chronic inflammation benefit significantly because A-Kavach™ directly targets “chemical arthritis.”
Why Timing Matters: The Earlier, the Better
By the time advanced arthritis appears on X-ray, a lot of cartilage is already lost. But the chemical destruction begins years earlier.
A-Kavach™ is your opportunity to intervene at the right time—not when the joint is already beyond biological rescue.
This is why early diagnosis and early biologic intervention are critical.
A-Kavach™ vs Conventional Arthritis Care
| Treatment | What It Does | Limitations |
|---|---|---|
| Painkillers | Reduce pain | Do not stop damage; may accelerate cartilage loss |
| Steroid injections | Quick relief | Short-term, can worsen long-term arthritis |
| Physiotherapy | Improves mechanics | Cannot neutralize biochemical attack |
| Knee replacement | Final-stage solution | Major surgery, not for early OA |
| A-Kavach™ | Targets chemical destruction + protects cartilage | Best in early and moderate OA |
The Science Behind the Shield
The A-Kavach™ protocol is rooted in:
- Mechano-biology
- Inflammation control
- Cartilage protection science
- Modulation of joint biochemical environment
- Understanding of pain-generation pathways
- Regenerative orthobiologic principles
This is a future-ready, precision-designed arthritis defence system.
Expected Outcomes With A-Kavach™
Most patients experience:
- Reduced pain and swelling
- Improved walking tolerance
- Better stair-climbing ability
- Increased knee confidence
- Reduced night pain
- Slowing of disease progression
- Delayed or avoided knee replacement
Because A-Kavach™ addresses root biochemical causes, not just symptoms.
Take the First Step Towards Joint Protection
Arthritis progression is not inevitable. The chemical assault can be slowed—sometimes dramatically—when addressed early and correctly.
A-Kavach™ is your biological shield. Let your knees fight back.
To learn more or book a consultation, visit:
www.orthobiologicsurgeryindia.com
www.drakvenkat.com