- PRASAD Treatment for Knee Osteoarthritis: What It Is, Who It Helps, and How It Works
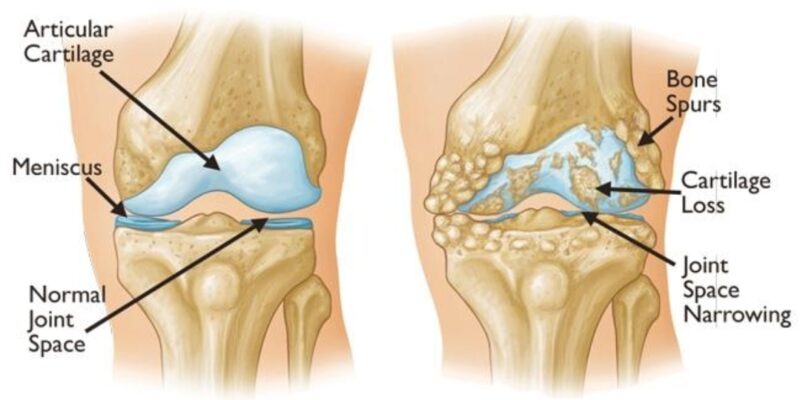
Most people believe knee osteoarthritis is simply a problem of worn-out cartilage. Modern research, however, shows that osteoarthritis is driven by chronic inflammation, metabolic imbalance, and altered cartilage cell behaviour.
The PRASAD Treatment was developed to address these deeper mechanisms. Rather than offering temporary pain relief, it aims to reset the joint’s biological environment so that function improves and disease progression slows.
Why Osteoarthritis Needs More Than Symptom Control
Osteoarthritis is now understood as a whole-joint disease involving cartilage, synovium, bone, muscles, and inflammatory signalling molecules. Persistent inflammation keeps the joint in a breakdown-dominant state, even when X-rays appear only mildly abnormal.
This explains why pain severity often does not correlate with imaging findings—and why isolated injections or painkillers rarely provide durable improvement.
What Is the PRASAD Treatment?
PRASAD is a structured regenerative protocol designed to:
- Reset chronic joint inflammation
- Improve cartilage and synovial metabolism
- Enhance the joint’s internal repair environment
- Restore strength-based load tolerance
- Delay or avoid knee replacement in selected patients
Unlike single-shot therapies, PRASAD is a phased protocol tailored to the patient’s inflammatory status, metabolic profile, and stage of osteoarthritis.
The Biological Rationale Behind PRASAD
Inflammation Reset
Stressed cartilage cells release danger signals known as alarmins. These molecules perpetuate inflammation and accelerate tissue breakdown. PRASAD targets this inflammatory loop to calm the joint before regenerative stimulation is applied.
Metabolic Rebalancing
In osteoarthritis, cartilage cells shift toward a catabolic (breakdown-driven) state. PRASAD incorporates metabolic correction and biologic modulation to push the joint environment back toward repair and stability.
Targeted Regenerative Support
Depending on patient selection, PRASAD may integrate platelet-based or cell-supported biologics, always within a controlled protocol rather than as stand-alone injections.
How PRASAD Differs From Standard Knee Injections
| Common Treatment | Primary Action | PRASAD Difference |
|---|---|---|
| Steroid injections | Short-term inflammation suppression | PRASAD avoids cartilage-weakening effects of repeated steroids |
| PRP | Growth factor delivery | Used only after inflammation is biologically controlled |
| Hyaluronic acid | Lubrication | PRASAD focuses on biological reset, not temporary viscosity |
Who Is an Ideal Candidate?
PRASAD is most effective for patients with:
- Early to moderate knee osteoarthritis
- Inflammatory flares with activity-related pain
- Stiffness that improves with movement
- Metabolic risk factors such as weight gain or insulin resistance
- A desire to delay or avoid knee replacement
Expected Outcomes
Patients commonly experience improvements in pain, swelling frequency, walking endurance, stair climbing, and confidence in knee function. Results are gradual but more durable because the underlying joint environment is altered.
Safety Considerations
PRASAD primarily uses autologous biologics combined with structured rehabilitation and metabolic correction. This results in a favourable safety profile when proper screening is followed.
Why PRASAD Represents the Future of Osteoarthritis Care
Modern osteoarthritis management is moving toward early biologic intervention, inflammation control, metabolic optimisation, and strength-based joint loading. PRASAD aligns with this evidence-driven direction.
For a simpler, patient-focused explanation of the PRASAD approach, read the detailed overview on drakvenkat.com.
Long-Term Follow-Up Update (2026)
We recently received a follow-up review from a patient who underwent our stromal-based biologic treatment 6 years ago.
They continue to report:
Sustained pain relief
Stable knee function
See the attached screen shots
Active daily lifestyle
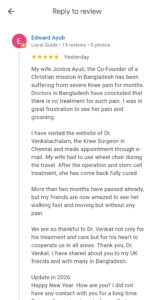
No need for knee replacement
- This long-term outcome reinforces the durability of biologic knee-preservation strategies when applied to appropriately selected patients.
Consultation
If you are exploring non-surgical regenerative options for knee arthritis, a personalised evaluation can determine whether the PRASAD protocol is appropriate for you.